Dr. Marian Fanica
2025 – present – general dentistry
CHARMDENTAL Dr. Enachescu, Ploiesti, Romania
Marian Fanica, DDS graduated from the University of Medicine and Pharmacy Carol Davila in Bucharest, Romania. He received a Bachelor’s Degree in Dentistry in 2005 and a Master’s Degree in Endodontics in 2015. His practice has been limited to Endodontics since 2015 with a field of interest also in Dental Adhesives. Marian is an international lecturer and hands-on dental trainer in Europe and Asia. His professional memberships include the European Association of Osseointegration, the Society of Esthetic Dentistry in Romania and the Dentistry National Organization in Romania.

Abstract
Successful retreatment of complex endodontic cases requires advanced skills and the use of specialized instruments. This case report details the management of a 52-year-old male presenting with severe pain associated with tooth 47, complicated by a significant periapical lesion and previous root canal therapy. The report highlights the clinical decision-making process, instrumentation strategies, and outcomes, emphasizing the importance of thorough debridement and careful restorative planning in endodontic retreatment.
Introduction
Endodontic retreatment presents unique challenges, particularly in cases of persistent infection, complex root canal anatomy, and previous inadequate therapy. The effective removal of filling materials and necrotic tissue is critical for healing and long-term success. This report describes a case involving teeth 47 and 16, focusing on the retreatment approach, instrumentation, and restoration.
Case Presentation
A 52-year-old male patient presented in 2021 with acute, severe pain localized to tooth 47 (mandibular right second molar). Clinical and radiographic examination revealed a large periapical lesion at tooth 47, despite the presence of a previous root canal treatment, and a compromised tooth 16 with extensive structural loss, subgingival decay, and perforation.
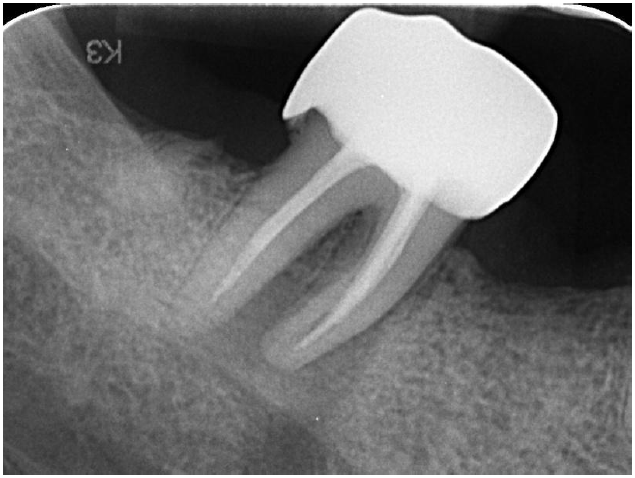
Large periapical lesion on tooth 47
Tooth 16 looks unsavable at this point
Treatment Procedure
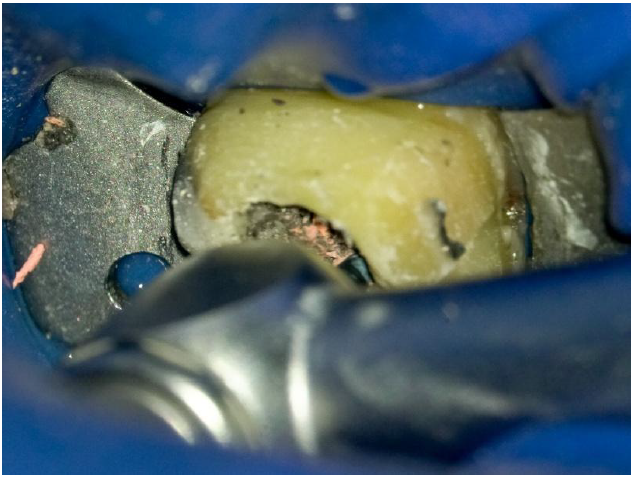
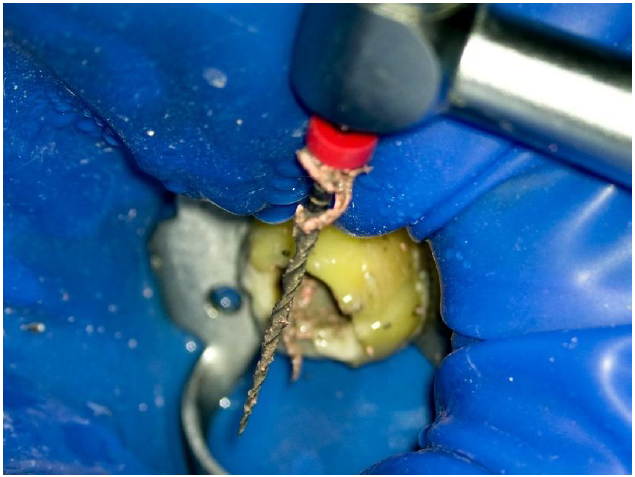
Following removal of the existing crown on tooth 47, retreatment was initiated using the Neoniti C1 file (450 RPM, 2.5 N·cm) and ultrasonic instruments to begin gutta-percha removal. The consistency of the gutta-percha resembled plastic, necessitating the use of Neolix files, which performed exceptionally in this scenario.

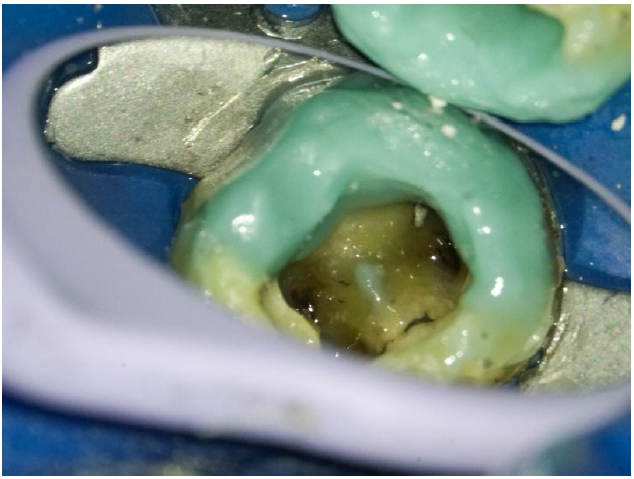
Aspect of the pulp chamber after removing the crown and coronal filling
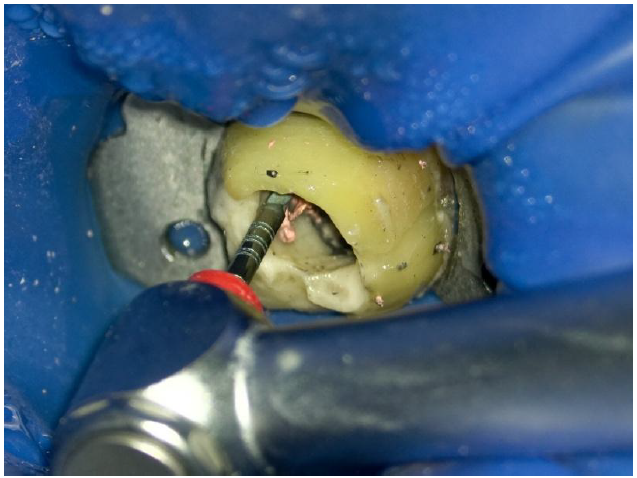
Treatment was initiated with Neolix Neoniti C1

Ultrasonic file used to remove gutta-percha, leveraging the “glide path” created by the file
Neoniti A1 25/06 employed as the primary retreatment instrument
The Neoniti A1 25/06 file (250 RPM, 1.5 N·cm) was instrumental in negotiating the canal to the apex. The process alternated between rotary files, ultrasonic files, Hedstrom hand files, and copious irrigation with sodium hypochlorite. Upon accessing the apex, a significant discharge of pus was observed, confirming the presence of an active periapical infection.

Neoniti A1 25/06 in use

Significant pus discharge from periapical lesion
Neoniti A1 25/06

Sodium hypochlorite irrigation

Even though I reached the apex, with 25/06, lots of gutta-percha remains on the root canal walls

It’s time now for ultrasound files to remove the rest of the gutta-percha
Radiographic evaluation revealed that the mesial root was primarily affected. The canal anatomy was complex, with a substantial isthmus connecting the mesiobuccal and mesiolingual canals, which had not been adequately cleaned in the previous treatment.

Hedstrom files employed to retrieve debris

Large isthmus with necrotic tissue visible between mesial canals
Restorative Phase
All existing composite restorations were removed to assess underlying structural integrity. Extensive decay was found beneath the lingual composite wall, which was subsequently restored using a contrast shade core build-up (Encore DC MiniMix) with a dual-cure adhesive (Connexio). Due to time constraints, calcium hydroxide was placed as an intracanal medicament before final obturation.

Decay present under the old composite filling
Restoring the lingual wall with contrast shade core build-up

Continuing the treatment

Placing calcium hydroxide as intermediate medication
Obturation and Follow-Up
In the subsequent session, final instrumentation was completed using the Neoniti 40/04 file in all canals. Root canal obturation was performed with a bioceramic sealer (NeoSEALER, Avalon).

Canals free from debris
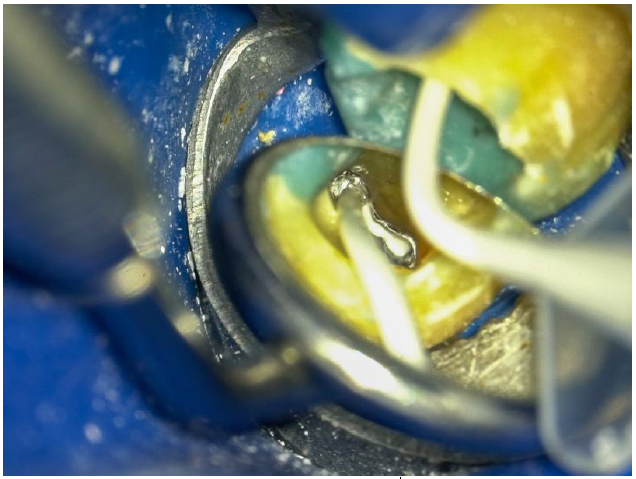
Application of bioceramic sealer
The old composite was etched with hydrofluoric acid to enhance adhesion and monoblock formation with the new material.
Dual-cure adhesives are mandatory when restoring with dual-cure or self-cure composites to prevent chemical incompatibility.
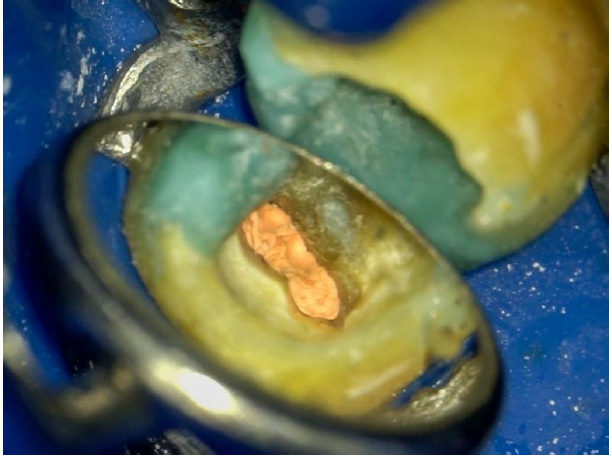
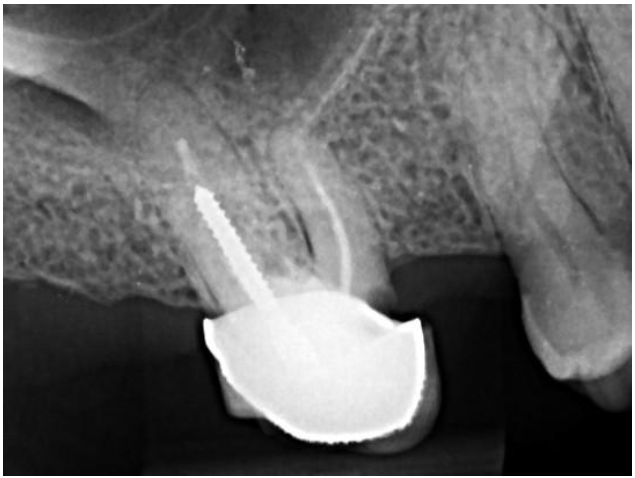
Image after compacting gutta-percha

Glass fiber post
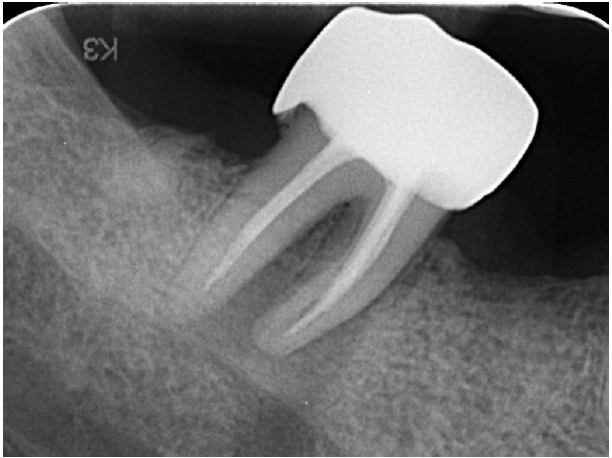
Radiograph with initial treatment
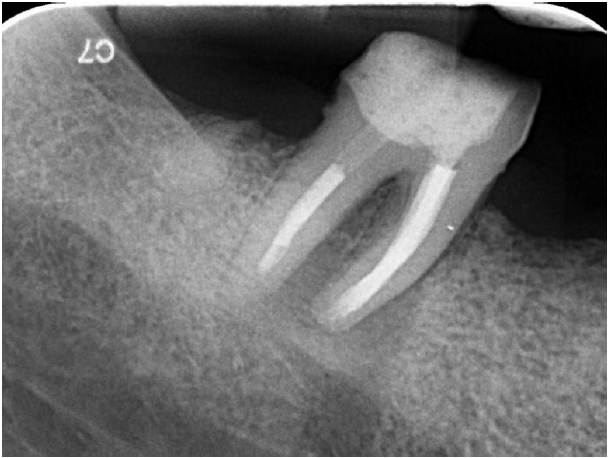
Radiograph after performing the retreatment
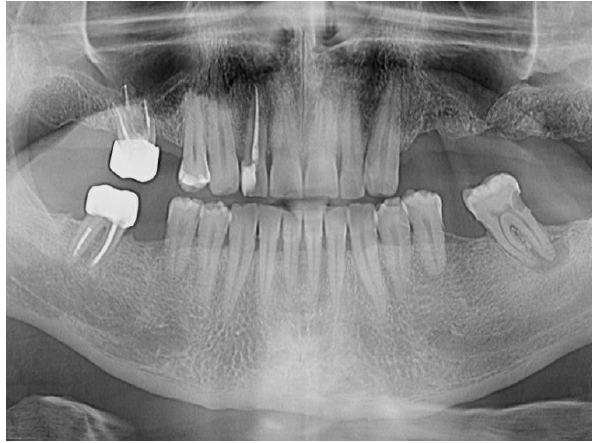
OPG shows great healing on 47 at 4 years follow-up
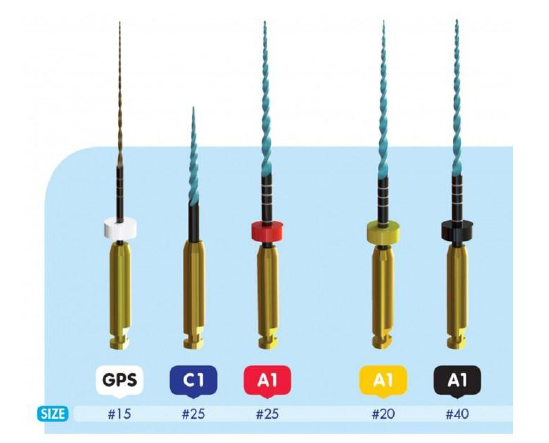
Files that made it possible
Discussion
This case underscores the necessity of tailored retreatment protocols, especially in teeth with complex root canal systems and persistent periapical pathology. The use of advanced rotary and ultrasonic instrumentation, combined with thorough irrigation and interim medication, facilitated successful debridement and healing. Radiographic assessment should be complemented by clinical evaluation of the apical seal.
Conclusion
Effective retreatment of challenging endodontic cases relies on detailed anatomical understanding, appropriate file selection, and meticulous cleaning strategies. The positive long-term outcome observed in this case demonstrates the value of modern retreatment techniques and comprehensive restorative management.
